Dizzy, tired, trouble focusing, abdominal symptoms, heart racing...
I'm hearing about all these concerns often so let's delve in!
These days I’m seeing an increase in just about any symptom you can think of.
It might simply be that it’s physical season and patients often come in with a list of questions that’ve built up over the year, but it’s also now well documented that many body systems are affected after recovering from an acute COVID infection. Most people have had at least one infection, so the rates of these concerns are rising.
Sidenote: It’s not a good idea to save up these concerns - each thing deserves its own time to evaluate at its own visit, but that’s not the subject of this post.
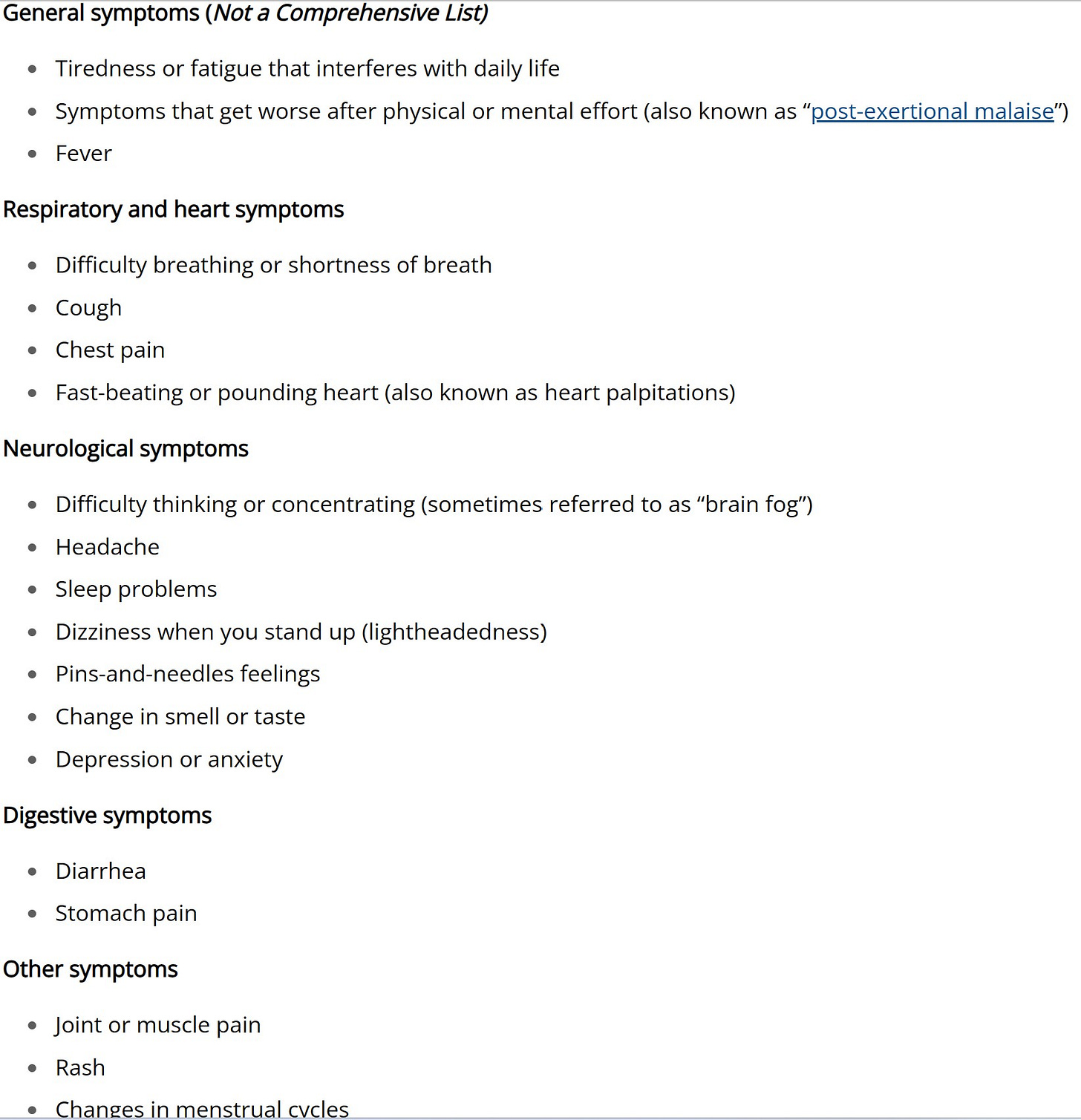
There are over 200 symptoms associated with post-COVID conditions. These don’t include the increase in chronic conditions, such as diabetes or epilepsy, often triggered by viral infections. From the CDC’s page on long COVID some of the most common are:
Feeling dismissed when you bring these symptoms up?
There’s a lot to be learned yet about the long term and late effects of a SARS-CoV2 infection.
We don’t have many tests to run or treatments to offer yet, but addressing the symptoms and looking for treatable causes is important.
Many lab and imaging studies are normal and aren’t always recommended, but that doesn’t mean there is not an underlying physical problem.
Too many people feel dismissed when their physician doesn’t have a treatment plan. I hope that no one feels dismissed when I don’t have a lot to offer. I simply don’t offer testing and treatment plans because there is not enough known yet about what should be done. Referring to specialists in the area of concern can be done, but the wait is often long and many report that the visit doesn’t answer questions. It’s frustrating for both the patient and the physicians involved.
Current recommendations
The CDC recommends eating well, managing stress, and getting accommodations for school if needed.
They also recommend joining support groups and getting involved in research to help identify better management plans.
They don’t offer anything specific because there aren’t specific tests or treatments known yet for most of the issues.
What might help.
I really like this booklet about autonomic dysfunction from the Mayo Clinic that I found on the Ehlers-Danlos Society page. (People with Ehlers-Danlos hypermobility syndrome are more commonly affected by autonomic dysfunction than others but anyone may be affected.)
The booklet explains in easy-to-understand detail what the autonomic nervous system is and how dysfunction affects some people. Autonomic dysfunction is not limited to post-covid conditions, but after COVID infections, many people seem to have symptoms consistent with it.
Autonomic dysfunction is often referred to as autonomic instability, dysautonomia, orthostatic intolerance, or POTS (postural orthostatic tachycardia syndrome). Blood flow problems, body temperature fluctuations, breathing difficulties, and digestion issues get out of balance when there is autonomic dysfunction. These can lead to a variety of problems sometimes seen after COVID or other viral infections.
People with autonomic dysfunction may have one or more of the following:
Dizziness/light-headedness or fainting
Fatigue (being tired all the time)
Headaches
Stomach pains or cramps
Nausea
Difficulty concentrating
Vision changes
Feelings of hot or cold
Excessive sweating
Increased heart rate
Chest pain
Leg weakness
Color changes in skin (blue or purple discoloration)
Mood changes (including anxiety or depression)
If you or someone you know has any of these symptoms, read the booklet from the Mayo Clinic and talk to your doctor. They can easily check heart rate and blood pressure laying and standing to see changes.
What if testing is normal but you think the results are wrong?
If the test is normal but you often have symptoms with changes in positioning, testing may need to be repeated under the right conditions. For example, if you have eaten salty snacks and are well hydrated and wearing compression clothing, you might not see orthostatic changes. Return for testing when you haven’t had a lot of salt or water and aren’t wearing compression socks or tight clothing for repeat testing. (Talk to your doctor before you purposefully restrict salt and water. You will be more likely to have symptoms, so it is best to not drive and to have someone walk with you in case you get faint or dizzy.)
If heart rate and blood pressure still don’t show changes, a tilt table test might be helpful.
Prevention is worth a pound of cure.
I am baffled why the world health leaders are not promoting the precautionary principle when it comes to all issues related to the pandemic since there is still so much unknown but there is growing evidence of long-term risk.
I know it can cause anxiety worrying about the potential problems, and many would prefer to just ignore it, but sometimes anxiety is good. It can help protect us from harm. As more and more people are suffering with long term effects after an infection, I’m hopeful that people start to take precautions against their next infection.
It would be ideal if we could use local infection risks to guide the numbers of precautions we take - much like we alter our clothing and activities based on the weather, we can add or remove protections based on local infection rates.
If you look at the year over year wastewater levels of SARS-CoV2, you can see that viral levels have been higher than other years many of the months so far this year. The pandemic isn’t over, it’s just changing over time.

Since there is so much unknown about the long term and late consequences of infection but more and more studies are showing ominous results, I think using precautions against getting infected (or reinfected) is important.
If you think the acute infections aren’t a big deal, did you know
studies show a persistence of replicating virus in many body organs, which can lead to lethal disease, even after asymptomatic and mild infections.
brain cells merge together into syncytia (making them permanently not work properly) as summarized by Dr. Eric Topol and discussed by Dr. Wes Ely.
immune system dysfunction contributing to more frequent infections with typical and atypical organisms (and no, masks won’t weaken the immune system - you don’t need to be exposed to infections that make you sick to keep your immune system working - that’s a very big misunderstanding popular on social media).
autoimmune problems rise after infections as summarized by Dr. Eric Topol.
developing either type 1 or type 2 diabetes is a risk following COVID infection.
seizure risk in adults and children increases after a COVID infection.
heart attack and stroke risks increase, even after mild infections.
the virus continues to mutate so it is possible to get reinfected many times with different variants - each potentially causing different damage.
immunizations seem to decrease the risk of both severe acute infections and long covid symptoms, but they do not fully prevent either.
It’s not over.
I’ve said for quite a while now that we’re living in a dystopian novel. How it will end is still unwritten. In the book there’s also the background of global warming, political unrest, racial and religious discrimination and intolerance, and other factors leading to the dystopian feel.
Chapter 1: everyone is scared and people everywhere are limiting interactions
Chapter 2: things are looking great with the vaccine
Chapter 3: despite ongoing viral infections and signs of long term problems people get back to living as if there’s no pandemic
Chapter 4 and beyond… yet to be written.
Maybe this is more like one of those books that you can choose the ending. If you use layers of precautions in response to current risks and try to live green, go to page 145. If you throw caution to the wind and fly to a big conference when there are a lot of sick people, go to page 321.
Long COVID Support Groups & more:
Long COVID Physio (adults)
Survivor Corps (adults)
Pacing guidelines for adult and pediatric people with long COVID: MEAction.net
Update 7/2/23
Dr. Ruth’s Substack has links to many new articles and studies highlighting my point above that the acute infection is just the start of the story.